Click on images and hypertext for expanded view. Click on ![]() for histology images.
for histology images.
Click on for pathology modules.
for pathology modules.
|
The Skeletal System | |
| Bones are the organs of the skeletal system. Functions of the
skeletal system are:
support - it forms the body's framework to support the muscles and organs. protection - the skeletal systems protects by 1) forming the bony cavities around organs, e.g. the thoracic cavity protects the heart and lungs, the cranial cavity protects the brain. 2) the red marrow in bones produces white blood cells which protect against invading microorganisms. movement - bones form joints which provide levers for movement such as walking, lifting, etc. hematopoiesis (blood cell production) - the red marrow produces both red and white blood cells. mineral storage and homeostasis - the skeleton forms a reservoir of minerals, especially calcium, for maintenance of homeostasis. | |
| Cells found in bone
tissue:
osteoprogenitor cells - these are like "stem cells" for bone. They have the capacity to divide and proliferate to form osteoblasts, bone forming cells which actively produce bone tissue. They comprise the periosteal and endosteal cells (see below) which line the bone and its cavities. In mature bone where growth and remodeling is not occurring these cells are quiescent, but they are thought to function in maintenance and nutritional support of the osteocytes in the underlying matrix, with which they connect by means of gap junctions. Osteoprogenitor cells are derived from mesenchymal cells (a fundamental embryological germ tissue) and have the ability to differentiate into adipose cells, chondroblasts, and fibroblasts and can modify their morphologic (physical) and physiologic characteristics in response to specific stimuli. osteoblasts - these are the "bone forming cells" which secrete the collagen and ground substance that constitutes unmineralized bone (osteoid), and subsequently are responsible for calcification of the matrix. These cells also communicate with one another and with osteocytes by gap junctions. Osteocytes are mature bone cells, differentiated from osteoblasts, which are responsible for maintaining the bone matrix. They can synthesize and resorb (break down) the matrix to maintain homeostasis. Each osteocyte occupies a space, the lacuna, which conforms to the shape of the cell surrounded by matrix secreted when the cell was an osteoblast. Osteocytes extend processes through canaliculi to connect to neighboring cells by means of gap junctions. Osteoclasts are large multinucleated cells whose function is to resorb bone. Osteoclasts dissolve the matrix and osteoid with acids and hydrolytic enzymes. Osteoclasts are phagocytic and are derived from monocytes and not from the same line as the other bone cells. | |
|
Tissues found in
bones:
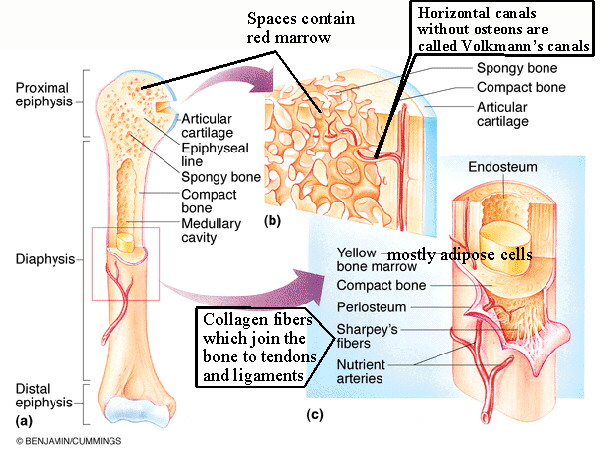
osseous tissues - bone tissue proper Osseous tissue has a matrix containing inorganic salts and organic fibers. The inorganic matrix gives the rigidity and hardness to bone and is composed of a combination of calcium and phosphorus salts called hydroxyapatite. The organic collagen fibers give a bone its tensile strength and resistance to stress. cortical (compact) bone - made of a dense regular arrangement of osteons (Haversian systems). Compact bone is found in the diaphysis (shaft) of long bones and as the outer layer of all bones. cancellous (spongy) bone - Consists of trabeculae (a network) of thin, connecting spicules which form a meshwork in the interior of bones. Spaces between the trabeculae contain marrow and blood vessels. red marrow - myeloid (blood producing) tissue found in the spaces in the spongy bone, produces both red and white blood cells. Red marrow does not increase in proportion to bone growth, and in the adult much of the red marrow changes to yellow (fatty) marrow, especially in the medullary canal. yellow marrow - Consists mostly of fat cells. It can revert to red marrow under extreme hematopoietic stress, such as in blood loss. periosteum - a fibrous covering of bones which connects to tendons and ligaments and anchors blood vessels and nerves. The inner layer of the periosteum contains osteoprogenitor cells, derived from mesenchyme cells, these are the cells which divide to become osteoblasts under appropriate stimuli. An extremely strong connection is formed with tendons and ligaments because the collagen fibers from these structures, called Sharpey's fibers, extend at an angle into the bone where they are continuous with collagen fibers in its extracellular matrix. endosteum - fibrous tissue lining the medullary canal. Often only once cells thick its cells are also osteoprogenitor cells. medullary canal - central canal of a long bone. It makes the bone lighter and in adults contains yellow marrow. articular cartilage - hyaline cartilage which forms part of synovial joints. |
 |
Osteons, or Haversian systems, are the units of structure in mature bone. They are tightly arranged running generally parallel to the long axis of the bone. At the center of each is an Haversian canal which carries blood vessels and nerves. Canaliculi (small canals) connect the Haversian canals with lacunae containing the osteocytes. Osteocytes extend processes into the canaliculi and receive nutrients and O2 and get rid of wastes and CO2 by diffusion through the canaliculi. The lacunae and canaliculi form lamellae or layers of two types: concentric lamellae form circular rings around each Haversian canal, and interstitial lamellae, derived from previous osteons, fill in the spaces between existing osteons. |
See Figure 6.7 |
Bone formation
(ossification): two types of bone development occur,
differentiated by whether membrane or cartilage is the precursor for the bone.
Subsequent remodeling of both types renders identical tissues for all bones.
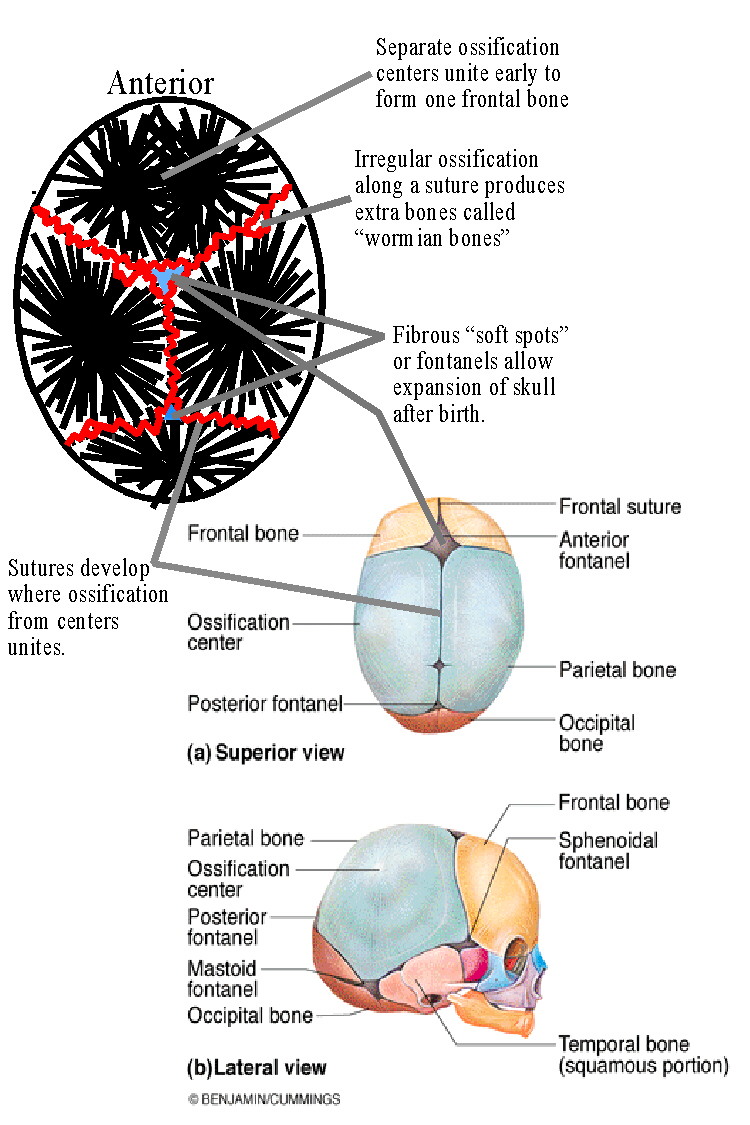
Intramembraneous ossification occurs in the flat bones such as those in the cranium and begins with a model of fibrous connective tissue. At about 8 weeks into development the mesenchymal cells aggregate and differentiate to become osteoblasts and begin the ossification process, first secreting the organic components of bone (osteoid, made of collagen and proteoglycans) as spikes radiating from an ossification center. Later inorganic salts will be deposited on the osteoid to form spicules of bone which form trabeculae in the general shape of the bone. Where the spikes meet irregular fibrous joints called sutures will be formed. Osteocytes extend their processes through canaliculi while new osteoprogenitor cells maintain the number of osteoblasts for continued growth of the bone spicules. |
| See Figure 6.8
|
Endochondral ossification is best exemplified in the long
bones. (See Figure 6.8):
1) Mesenchymal cells aggregate and differentiate into chondroblasts which
produce
a model of hyaline cartilage that precedes each bone. At about 8 weeks into
development cells in the mid-region begin to differentiate into osteoblasts which
produce a thin layer of bone around the cartilage model. In long bones a bone collar
develops around what will become the shaft (diaphysis). 2) Cartilage cells in
the
center hypertrophy and cause calcification of the matrix, and then die as they
become isolated from their nutrient source. With the death of the chondrocytes the
matrix breaks down resulting in early formation of the marrow cavity. 3) By
the
third month blood vessels called the periosteal bud invade the developing
cavity
bringing in osteoprogenitor cells and other cells and spongy bone and marrow
begins to form. 4) At birth the long bones consist of a collar of cortical bone
along
the shaft and a developing medullary canal. Secondary ossification centers form in
the epiphyses which push outward and to the center while osssification continues
along the diaphysis toward the epiphyses. 5) Ossification of the epiphyses.
The
proximal end begins near birth and continues until 18 or 19 yrs. of age. The distal
end begins 1 to 1.5 years old and continues until the early 20's, although all
substantial growth has ended in the late teens.
The only remaining cartilage is in the epiphyseal plate and the articular cartilage. Bone growth stops when the epiphyseal plate hardens. |
| Bone Remodeling:
Your bones are constantly remodeled throughout your life. This process helps to keep them strong and to maintain their integrity for withstanding stresses, and maintaining homeostasis. The process involves first osteoclastic resorption of an area of bone ,and then subsequent capillary penetration and osteoblastic action to produce a new osteon. In a healthy adult the rate of resorption roughly equals the rate of bone deposition. In older people the rate of deposition often falls below that of resorption and osteoporosis results. Bone remodeling is stimulated by physical stress placed on the bone by exercise, and will be tailored to provide specific adaptation to that stress. In that way a weight lifter's bones will show growth patterns peculiar to the stresses placed on the bones. | |
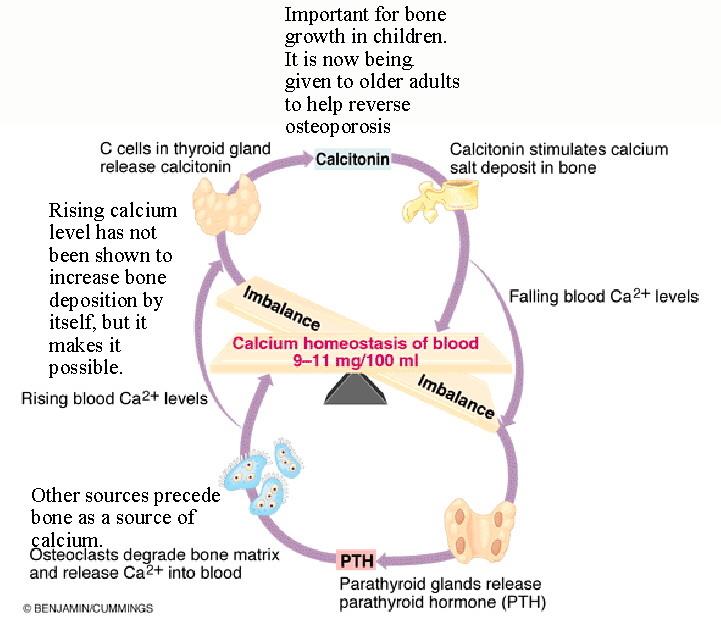 |
Hormones important to bone growth and homeostasis:
growth hormone - from the anterior pituitary, this hormone is necessary for normal growth and development of the skeleton. A deficiency (hyposecretion) of GH during childhood produces a dwarf, an excess (hypersecretion) produces a giant. Hypersecretion in adulthood produces acromegaly, a disorder in which the shape of many bones, especially those in the face becomes exaggerated. thyroxine - this hormone, actually its active product, regulates metabolism of most cells including those in bone. testosterone - this and other androgens are important for growth in mass and density of bone. Testosterone is present in both males and females in varying amounts. estrogens - these hormones are important for growth in length of bone and for bone maintenance. They too are present in varying amounts in both sexes. parathyroid hormone - this hormone exerts the primary control in calcium homeostasis. Calcium is necessary in the blood for many functions and when its level falls parathyroid hormone is secreted. This hormone uses several methods to raise calcium levels in the blood: 1) increased Vitamin D production. Vitamin D is a hormone whose precursor is produced in the skin in response to sunlight and then processed in the liver and kidney to become active Vitamin D3. 2)Vitamin D3 increases calcium absorption in the gut. Without this vitamin calcium is not absorbed to any great degree. 3) increased reabsorption of calcium in the kidney. Much calcium is lost to the urine, so when you need more in the blood this is an important source. 4) resorption of bone. PTH increases osteoclastic activity to release calcium into the blood. Calcitonin - Normally important only in children, this hormone is secreted by special cells in the thyroid. Its function is to stimulate the uptake of calcium into growing bone and the deposition of bone matrix. It has been used in adults to aid in the uptake of calcium in osteoporosis patients. |
| Osteoporosis, a disorder involving
demineralization of bone usually associated with older individuals
can be related to several factors:
1) deficiency of dietary calcium 2) reduced estrogen levels common in post-menopausal women. This may be treated with HRT, hormone replacement therapy. 3) reduced activity and exercise, including: 4) reduced weight bearing stress on the bones. This is important in stimulating bone growth and replacement at any age. Osteoporosis treatment may include calcium formulated with other minerals, hormone replacement therapy, calcitonin, and an exercise program. Other disorders: rickets - Vitamin D deficiency in children. Vitamin D is necessary for absorption of calcium. The result of rickets is improper mineralization which results in stunted growth and weakened bones. osteomalacia - Vitamin D deficiency in adults. Causes demineralization of the bones. Paget's disease - a disorder of unknown cause which involves the
destruction of normal bone tissue and
its replacement with tissue of irregular and unorganized structure.
| |
NOTE: These notes do not include the bones and contours you are required to know (See Short List of Bones and Contours). Instructor will go over many of these in class, depending on time available.